What It Is
What is a knee replacement?
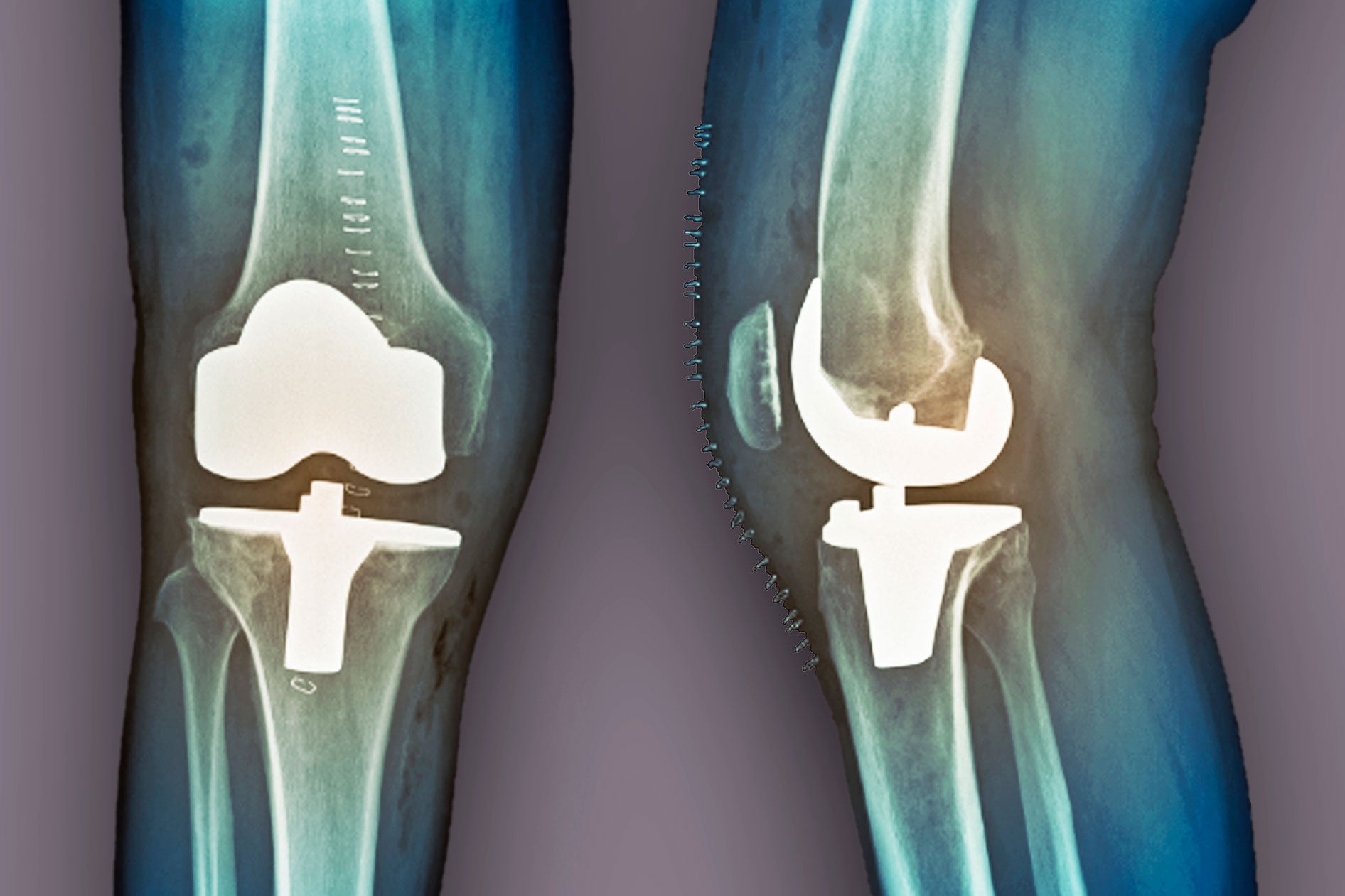
A knee replacement is surgery to remove a damaged knee joint and replace it with an artificial joint, or knee implant. Your knee joint is made up of your thigh bone, shinbone and kneecap. It also contains soft tissues like cartilage. The goal of knee replacement is to restore pain-free range of motion and full knee function.
Knee replacement is common, but orthopedic knee surgery comes with risks and potential complications. Consider getting a second opinion about all your treatment choices, including nonsurgical options, before deciding on knee replacement.
Types of knee replacement include:
-
Total knee replacement removes the entire knee joint.
-
Partial knee replacement only removes one side of the affected joint. Unicompartmental knee replacement is another name for this procedure. When only one of the three knee compartments is diseased, this may be an alternative to a total knee replacement.
Why It's Done
Why is knee replacement performed?
Your doctor may recommend knee replacement for severe knee joint damage from:
-
Knee injuries including fractures, torn cartilage, and damage to ligaments or tendons resulting in irreversible joint damage
-
Osteoarthritis (degenerative joint disease). This breakdown of cartilage and bones within the joint results in pain, stiffness and swelling. It is the most common reason for a knee replacement.
-
Rheumatoid arthritis and other inflammatory causes of arthritis
-
Septic arthritis (infection in the joint space)
Your doctor may only consider a knee replacement if other treatment options that involve less risk of complications have been ineffective. Your personal risk of complications depends on your age, knee anatomy, and overall health. Talk with your doctor about your risks and ask if the benefits of surgery outweigh the risks.
Who to See
Who performs knee replacement?
An orthopedic surgeon performs knee replacement. An orthopedic surgeon has specialized training in the surgical treatment of diseases and conditions of the bones and connective tissues. Some orthopedic surgeons further specialize in joint reconstruction and replacement, or in knee surgery specifically. Experience is critically important when you are choosing a knee replacement surgeon. Ask your orthopedic surgeon about the types and volume of surgeries she performs on a monthly basis over the past several years.
How It's Done
How is knee replacement performed?
Knee replacements are performed in hospitals and orthopedic surgery centers. A knee replacement can either be an open or minimally invasive procedure. Open knee replacement surgery requires an 8- to 10-inch incision over your knee to expose the whole joint and place the knee implant. With minimally invasive knee replacement (arthroscopic knee replacement), your surgeon makes a 4- to 6-inch incision. In general, partial knee replacements typically require a smaller incision than total knee replacements.
Open procedures are the traditional method of performing a knee replacement. However, minimally invasive surgery, as compared to an open procedure, generally entails a faster recovery time, less pain, and a lower risk of some complications, such as infection.
In some cases, your doctor may combine a minimally invasive procedure with an open surgery. In addition, your doctor may decide after beginning a minimally invasive technique that open surgery is necessary to safely and most effectively complete your surgery. Your surgeon may also decide after beginning a partial knee replacement that a total knee replacement is a better option for you. Discuss these possibilities with your doctor before surgery.
Your doctor will explain which procedure is best for you—total or partial, and open or arthroscopic knee replacement—based on your diagnosis, age, medical history, general health, and possibly your personal preference.
Types of anesthesia that may be used
Your doctor will use either general anesthesia or regional anesthesia.
-
General anesthesia is a combination of intravenous (IV) medications and gases that put you in a deep sleep. You aren’t aware of the surgery and don’t feel any pain. Some surgeons include a peripheral nerve block infusion with general anesthesia. The anesthetic flows through a tiny tube inserted near your surgical site to control pain during and after surgery.
-
Regional anesthesia, or nerve block, is an injection of anesthetic around certain nerves to numb a large area of the body. A femoral nerve block to numb most of the leg is one of the more common nerve blocks for knee surgery. You will most likely have a sedative to keep you relaxed and comfortable.
What to expect the day of your knee replacement
In general, this is what happens the day of your surgery:
-
Talk with a preoperative nurse, who will make sure you understand and sign the surgical consent form.
-
Change into a hospital gown. It is a good idea to leave all jewelry and valuables at home or with a family member.
-
Talk with the anesthesiologist or nurse anesthetist about your medical history and the type of anesthesia you will have.
-
A surgical team member will start an IV.
-
The anesthesiologist or nurse anesthetist will start your anesthesia.
-
A tube may be placed in your windpipe to protect and control your breathing during general anesthesia.
-
The surgical team will monitor your vital signs and other critical body functions. This occurs throughout the procedure and your recovery until you are alert, breathing effectively, and your vital signs are stable.
Risks and Complications
What are the risks and potential complications of knee replacement?
As with all surgeries, both partial and total knee replacement surgery involves risks and potential complications. Complications may become serious and life threatening in some cases.
General risks of surgery
The general risks of surgery include:
-
Anesthesia reaction, such as an allergic reaction and problems with breathing
-
Bleeding, which can lead to shock
-
Blood clot, in particular a deep vein thrombosis that develops in the leg or pelvis. It can travel to your lungs and cause a pulmonary embolism.
-
Infection
Potential complications of knee replacement
Most knee replacements are successful, but potential complications include:
-
Dislocation of the new joint
-
Loosening of the new joint, which may require additional surgery to secure the new joint and relieve pain
-
Nerve, muscle, or blood vessel damage
-
Wear and tear of the new joint, which may eventually lead to another knee replacement surgery
Reducing your risk of complications
You can reduce your risk of certain complications by:
-
Following activity, dietary and lifestyle restrictions and recommendations before your surgery and during recovery
-
Informing your doctor if you are nursing or if there is any possibility of pregnancy
-
Notifying your doctor immediately of any concerns, such as bleeding, fever, or increase in pain
-
Taking your medications exactly as directed
-
Telling all members of your care team if you have allergies
How to Prepare
How do I prepare for knee replacement?
The steps you take before surgery can improve your comfort and outcome. You can prepare for a knee replacement by:
-
Answering all questions about your medical history, allergies, and medications you take. This includes prescriptions, over-the-counter drugs, herbal treatments, and vitamins. It is a good idea to carry a current list of your medical conditions, medications, and allergies at all times.
-
Getting preoperative testing as directed. Testing will vary depending on your age, health, and specific procedure. Preoperative testing may include a chest X-ray, EKG (electrocardiogram), blood tests, and other tests as needed. These tests help ensure you are in good overall health for surgery.
-
Losing excess weight before surgery through a healthy diet and exercise plan.
-
Not eating or drinking before surgery as directed. Your surgery may be cancelled if you eat or drink too close to the start of surgery because you can choke on stomach contents during anesthesia.
-
Stopping smoking as soon as possible. Even quitting for just a few days can be beneficial and help the healing process.
-
Taking or stopping medications exactly as directed. This may include not taking aspirin, ibuprofen (Advil, Motrin), and blood thinners. Your doctor will give you instructions for taking your specific medications and supplements.
Questions to ask your doctor
Facing surgery can be stressful. It is common for patients to forget some of their questions during a doctor’s office visit. You may also think of other questions after your appointment. Contact your surgeon/doctor with concerns and questions before surgery and between appointments.
It is also a good idea to bring a list of questions to your preoperative appointments. Questions can include:
-
Why do I need a knee replacement? Are there any other options for treating my condition?
-
What type of knee replacement procedure will I need?
-
Am I a good candidate for a partial knee replacement? How many partial knee replacements have you performed?
-
How long will the procedure take? When will I be able to go home?
-
How frequently do you encounter complications from the surgery? Do you have outcomes data you can share with me?
-
What restrictions will I have after the surgery, and when can I expect to return to work and other activities?
-
What kind of assistance will I need at home?
-
What medication plan should I follow before and after the surgery?
-
How will my pain be managed?
-
When and how should I contact you? Ask for numbers to call during and after regular hours.
What to Expect
What can I expect after my knee replacement?
Knowing what to expect makes it easier to plan and prepare for a successful recovery.
How long will it take to recover?
You will stay in the recovery room after surgery until you are alert, breathing effectively, and your vital signs are stable. You may have a sore throat if a tube was placed in your windpipe during surgery. This is usually temporary, but tell your care team if you are uncomfortable.
A knee replacement usually requires a hospital stay of several days. The stay after a partial knee replacement is typically shorter—1 to 3 days. In some cases, you may need to stay in a rehabilitation center after you are discharged from the hospital to help you safely return home.
Recovery time varies depending on the procedure, type of anesthesia, your general health, age, and other factors. It will probably be 2 to 3 months before you're feeling back to normal. Full recovery and range of motion can take 3 to 12 months.
Physical therapy is an essential part of recovery. It begins very soon after surgery, even during hospitalization. Gradually, you’ll regain knee function with less pain.
Will I feel pain?
Your doctor will prescribe a course of pain medication as well as over-the-counter (OTC) pain relievers so you are comfortable and can get the rest you need. The key to pain control is to take your pain meds—both prescription and OTC—as your doctor prescribes or according to package directions. Staying ahead of the pain is important for healing and a smooth recovery. It will also help you keep up with physical therapy.
When should I call my doctor?
It is important to keep your follow-up appointments after a knee replacement. Contact your doctor for questions and concerns between appointments. Call your doctor right away or seek immediate medical care if you have:
-
Bleeding
-
Breathing problems, such as shortness of breath, difficulty breathing, labored breathing, or wheezing
-
Change in alertness, such as passing out, unresponsiveness, or confusion
-
Chest pain, chest tightness, chest pressure, or palpitations
-
Fever. A low-grade fever (lower than 101 degrees Fahrenheit) is common for a couple of days after surgery. It is not necessarily a sign of a surgical infection. However, you should follow your doctor's specific instructions about when to call for a fever.
-
Inability to urinate or have a bowel movement
-
Leg pain, redness or swelling, especially in the calf, which may indicate a blood clot
-
Numbness or tingling in the affected extremity
-
Pain that is not controlled by your pain medication
-
Unexpected drainage, pus, redness or swelling of your incision
How might a knee replacement affect my everyday life?
A knee replacement can significantly improve your mobility so you can lead an active life without knee pain. With a partial knee replacement, it is possible to have continued pain or to develop problems in the other knee compartments.
In most cases, a knee replacement results in very few limitations or restrictions to your daily routine. You might even be able to enjoy activities that you had to stop before surgery. To extend the life of your knee implant, your doctor may recommend avoiding:
-
Activities that could overload your knees, such as heavy lifting
-
Contact sports and high-impact activities
-
Sports that require you to move laterally, such as skiing or tennis
Your doctor will discuss specific limitations with you. Keep in mind that any restrictions you have may ease with time as your leg strength improves.