What It Is
What is a total hip replacement?
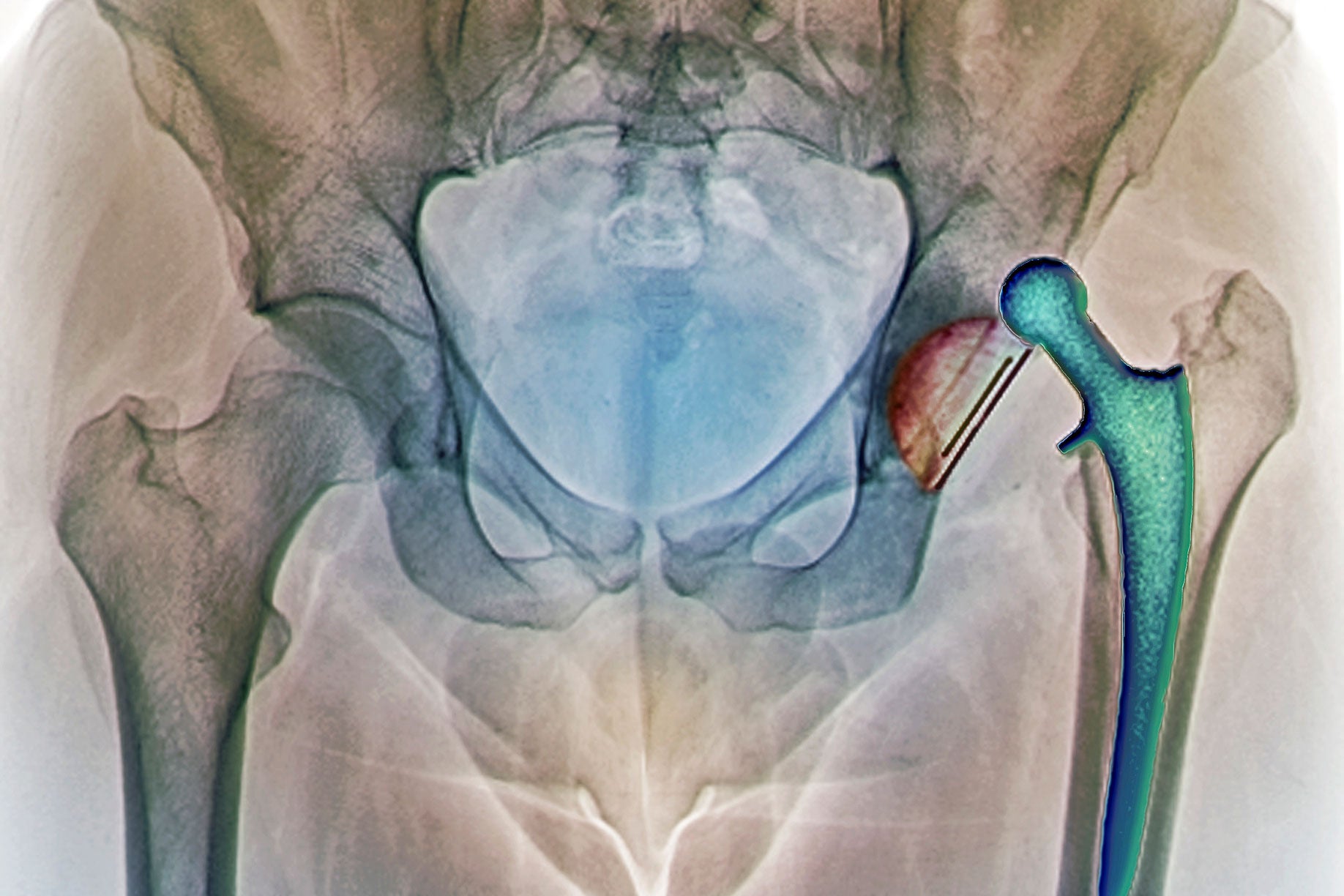
A total hip replacement is the surgical removal of the entire hip joint and replacement with an artificial joint called a prosthesis. Your hip joint is formed where your thigh bone (femur) and your hip bone (pelvis) meet. It is a ball and socket joint. The ball-shaped area at the top of your femur fits into a socket-shaped area in your pelvis. Your hip joint also contains ligaments, tendons, cartilage, and lubricating fluid.
Total hip replacement can help restore pain-free range of motion and function in a hip joint damaged by arthritis, injury, or other hip problems.
A total hip replacement is a common but major surgery with significant risks and potential complications. You may have less invasive treatment options. Consider getting a second opinion about treatment options before having a total hip replacement.
Types of total hip replacement
The types of total hip replacement procedures include:
-
Cemented replacement involves special surgical cement to attach the prosthesis to your bone. This procedure is often appropriate for older, less active people or people with weakened bones.
-
Uncemented replacement uses a prosthesis with a special coating that promotes bone growth into the prosthesis. This procedure has a longer recovery period because it takes time for your bone to grow and securely attach the prosthesis. This bone growth also tends to cause more thigh pain in the months after surgery. Uncemented prostheses are usually more appropriate for younger, active people.
-
Hybrid replacement involves a combination of cemented and uncemented prostheses. Usually, the femur (ball) part of the prosthesis is cemented and the pelvic (socket) part of the prosthesis is uncemented.
Why It's Done
Why is a total hip replacement performed?
Your doctor may recommend hip replacement to treat a variety of diseases and conditions of the hip. Your doctor may only consider a total hip replacement if other treatment options with less risk of complications are not working. Ask your doctor about all of your treatment options and consider getting a second opinion before deciding on hip replacement.
Your doctor may recommend hip replacement for severe hip joint damage and pain caused by:
-
Bone tumors, which can cause breakdown of the bone
-
Hip joint infections, also called septic arthritis
-
Hip joint injuries including fractures, torn ligaments, and torn cartilage, which may lead to irreversible joint damage
-
Osteoarthritis, or degenerative joint disease. This is the breakdown of cartilage and bones within the joint, resulting in pain, stiffness and swelling. It is the most common reason for a total hip replacement.
-
Osteonecrosis, a rare condition involving death of bone
-
Rheumatoid arthritis, an autoimmune disease characterized by joint inflammation
Who to See
Who performs a total hip replacement?
An orthopedic surgeon will perform your total hip replacement. An orthopedic surgeon specializes in surgical treatment of diseases of the bones and connective tissues.
How It's Done
How is a total hip replacement performed?
Your surgeon will perform your hip replacement in a hospital or surgical center using one of the following approaches:
-
Minimally invasive surgery involves inserting special instruments and an arthroscope through one (three to six inch) or two (two to three inch) incisions in your hip. An arthroscope is a thin, lighted instrument with a small camera. The camera transmits pictures of the inside of your body to a video screen viewed by your doctor as he or she performs the surgery. Minimally invasive surgery generally involves a faster recovery and less pain than open surgery. This is because it causes less damage to tissues and muscles. Your surgeon will make small incisions instead of a larger one used in open surgery. Your surgeon threads surgical tools around structures and muscles instead of cutting through or displacing them as in open surgery.
-
Open surgery involves making a large 10- to 12-inch incision in your hip. An open surgery incision allows your doctor to directly view and access the surgical area. Open surgery requires a larger incision and involves more cutting and displacement of muscle and other tissues. Open surgery generally involves a longer recovery and more pain than minimally invasive surgery because it causes more damage to tissues. Despite the potential for damage, open surgery may be a safer or more effective method for certain patients.
Your doctor will determine which type of surgery is best for you and how long you need to stay in the hospital or surgical center based on your diagnosis, age, medical history, general health, and possibly your personal preference. Learn about the different total hip replacement procedures and ask why your doctor will use a particular type of procedure for you.
Types of anesthesia that may be used
Your surgeon will perform a total hip replacement using either regional anesthesia or general anesthesia, depending on the specific procedure.
-
General anesthesia is a combination of intravenous (IV) medications and gases that put you in a deep sleep. You are unaware of the procedure and will not feel any pain. You may also receive a peripheral nerve block infusion in addition to general anesthesia. A peripheral nerve block infusion involves an injection or a continuous drip of a liquid anesthetic. The anesthetic flows through a tiny tube inserted near your surgical site to control pain during and after surgery.
-
Regional anesthesia is also known as a nerve block, an epidural, or spinal anesthesia. Your anesthesiologist or nurse anesthetist will inject an anesthetic around certain nerves in the spine so you do not feel anything from the waist down. You will likely have sedation with regional anesthesia to keep you relaxed and comfortable.
What to expect the day of your total hip replacement
The day of your surgery, you can generally expect the following:
-
Talk with a preoperative nurse. The nurse will perform an exam and ensure that all needed tests are in order. The nurse can also answer questions and will make sure you understand and sign the surgical consent.
-
Remove all clothing and jewelry and dress in a hospital gown. It is a good idea to leave all jewelry and valuables at home or with a family member if possible. The surgical team will give you blankets for modesty and warmth.
-
Talk with the anesthesiologist or nurse anesthetist about your medical history and the type of anesthesia you will receive.
-
A surgical team member will start an IV.
-
The anesthesiologist or nurse anesthetist will start your anesthesia.
-
A tube will be placed in your windpipe to protect and control your breathing during general anesthesia. A catheter will be inserted into your bladder to drain urine and monitor kidney function. You will not feel or remember these procedures or the surgery.
-
The surgical team will monitor your vital signs and other critical body functions. This occurs throughout the procedure and recovery until you are alert, breathing effectively, and your vital signs are stable.
Risks and Complications
What are the risks and potential complications of a total hip replacement?
As will all surgeries, hip replacement surgery involves risks and potential complications. Complications may become serious and life threatening in some cases. Complications can develop during the procedure or throughout your recovery.
General risks of surgery
The general risks of surgical procedures include:
-
Anesthesia reaction, such as an allergic reaction and problems with breathing
-
Bleeding, which can lead to shock or the need for blood transfusions.
-
Blood clot, in particular a deep vein thrombosis. A blood clot can travel to your lungs and cause a pulmonary embolism. Blood clots in the legs or pelvis are the most common complication of hip replacement surgery. To prevent this, your doctor may prescribe blood thinning medication, support hose, inflatable leg coverings, or ankle pump exercises.
- Infection
Potential complications of hip replacement
Complications of hip replacement can be serious and include:
-
Abnormal bone growth
-
Continued or worsened pain
-
Dislocation of the new joint
-
Joint stiffness
-
Loosening of the new joint causing pain and the possibility of additional surgery to secure the new joint
-
Nerve, muscle, or blood vessel damage
-
Uneven leg lengths may occur or worsen after a total hip replacement. Shoe lifts can help offset this complication.
-
Wear and tear of the new joint requiring another replacement
Reducing your risk of complications
You can reduce the risk of certain complications by following your treatment plan and:
-
Following activity, dietary and lifestyle restrictions and recommendations before surgery and during recovery
-
Notifying your doctor immediately of any concerns, such as bleeding, fever, increase in pain, or wound redness, swelling or drainage
-
Taking your medications exactly as directed
-
Telling all members of your care team if you have any allergies
How to Prepare
How do I prepare for my total hip replacement?
You are an important member of your own healthcare team. The steps you take before surgery can improve your comfort and outcome. You can prepare for a total hip replacement by:
-
Answering all questions about your medical history and medications you take. This includes prescriptions, over-the-counter drugs, herbal treatments, and vitamins. It is a good idea to carry a current list of your medical conditions, medications, and allergies at all times.
-
Getting preoperative testing as directed. Testing varies depending on your age, health, and specific procedure. Preoperative testing may include a chest X-ray and other imaging tests, EKG (electrocardiogram), blood tests, and other tests as needed.
-
Informing your doctor or radiologist if you are nursing or if there is any possibility that you may be pregnant
-
Losing weight before the surgery through a healthy diet and exercise plan
-
Not eating or drinking just prior to surgery as directed. Your doctor may cancel your surgery if you eat or drink too close to the start of the procedure because you can choke on stomach contents during anesthesia.
-
Stopping smoking as soon as possible. Even quitting for just a few days can be beneficial and help the healing process.
-
Taking or stopping medications exactly as directed. For a total hip replacement, this may include not taking aspirin, ibuprofen (Advil, Motrin), and blood thinners.
Questions to ask your doctor
Facing surgery can be stressful. It is common for patients to forget some of their questions during a doctor’s office visit. You may also think of other questions after your appointment. Contact your doctor with concerns and questions before surgery and between appointments.
It is also a good idea to bring a list of questions to your preoperative appointments. Questions can include:
-
Why do I need a total hip replacement? Are there any other options for treating my condition?
-
What type of total hip replacement procedure will I need?
-
How long will the procedure take? When can I go home?
-
What kind of restrictions will I have after the surgery? When can I return to work and other activities?
-
What kind of assistance will I need at home?
-
What type of physical therapy or rehabilitation will I need?
-
What medications will I need before and after the surgery? How should I take my usual medications?
-
How will you manage my pain?
-
When should I follow up with you?
-
How should I contact you? Ask for numbers to call during and after regular hours.
What to Expect
What can I expect after my total hip replacement?
Knowing what to expect can help make your road to recovery after a total hip replacement as smooth as possible.
How long will it take to recover?
You will stay in the recovery room after surgery until you are awake, alert, and your vital signs are stable. You may have a sore throat if a tube was placed in your windpipe during surgery. This is usually temporary, but tell your care team if you are uncomfortable. You may also have a small tube (drain) in your incision to help drain fluids. Your surgeon will remove this before you leave the hospital.
You may need to use crutches or a walker for several days after your surgery. A physical therapist will help you to begin walking the day after the surgery. You will also learn exercises to strengthen the hip, and how to properly use your new hip joint. You may also wear special stockings to prevent blood clots. If you are at high-risk of developing blood clots in the legs, you may receive a blood thinner. A respiratory therapist will teach you deep breathing exercises to help prevent pneumonia.
A hospital stay of three to five days may be required. You may also need to stay in a rehabilitation center after your discharge from the hospital. This will help you improve your mobility and joint function so you can safely return home.
Recovery after surgery is a gradual process. Recovery time varies depending on the specific procedure, type of anesthesia used, your general health, age, and other factors. Full recovery times range from three to six months.
Will I feel pain?
Pain control is important for healing and a smooth recovery. There will be discomfort after your surgery. Your doctor and care team will manage your pain so you are comfortable and can get the rest you need. Contact your doctor if your pain gets worse or changes because it may be a sign of a complication, such as infection.
When should I call my doctor?
It is important to keep your follow-up appointments after a total hip replacement. Call your doctor if you have concerns or questions between appointments. Call your doctor right away or seek immediate medical care if you have:
-
Bleeding
-
Breathing problems, such as shortness of breath, difficulty breathing, labored breathing, or wheezing
-
Change in alertness, such as passing out, dizziness, unresponsiveness, or confusion
-
Chest pain, chest pressure or chest tightness
-
Cough
-
Fever. A low-grade fever (lower than 101 degrees Fahrenheit) is common for a couple of days after surgery and not necessarily a sign of a surgical infection. However, you should follow your doctor's specific instructions about when to call for a fever.
-
Inability to urinate or have a bowel movement
-
Leg pain, redness or swelling, especially in the calf, which may indicate a blood clot
-
Numbness or tingling in the affected leg
-
Pain that is not controlled by your pain medication or pain that gets worse or changes
-
Unexpected drainage, pus, redness or swelling of your incision
How might a total hip replacement affect my everyday life?
Total hip replacement may cure your condition or reduce your symptoms so you can lead an active, normal life. For example, hip replacement may relieve your pain and restore range of motion to your hip. However, hip replacement can also cause significant changes to your body that affect your everyday life and require you to:
-
Avoid contact sports and sports requiring lateral movements, such as downhill skiing or tennis
-
Avoid high-impact activities, such as running and jumping
-
Notify your dentist that you have had a total hip replacement. You may need to take antibiotics before dental procedures.
-
Participate in low-impact sports, such as walking, swimming, cross country skiing, or stationary biking
-
Practice strength training and range-of-motion exercises as recommended by your healthcare provider
-
Taking extra precautions to avoid falls and injuries